Healthcare worker screening with QFT-Plus
Healthcare workers are at 2- to 5-fold increased risk of developing latent TB infection compared with the general population (1). Even employees with brief patient contact and members of staff without patient care responsibilities may be exposed to TB through droplets from a person with TB disease. Transmission of TB bacteria in healthcare settings to and between patients and healthcare workers has been reported in virtually every country of the world, regardless of how much TB exists in the local community.
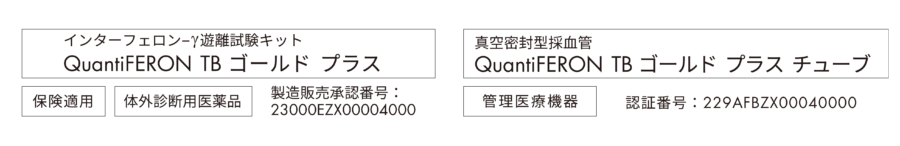
QuantiFERON-TB Gold Plus (QFT-Plus) is an indirect blood test that can help detect TB infection. QFT-Plus is a major scientific advance over the 100-year-old tuberculin skin test (Mantoux, TST, or PPD), giving greater accuracy and cost-effectiveness, and a more reliable result in a single visit.

QFT-Plus advantages compared to the tuberculin skin test for healthcare worker testing
| Characteristic | Tuberculin skin test (TST) | QuantiFERON-TB Gold Plus (QFT-Plus) |
|---|---|---|
| Single patient visit | NO | YES |
| Use of positive and negative controls | NO | YES |
| Objective results | NO | YES |
| Unaffected by BCG vaccination | NO | YES |
| Unaffected by most environmental non-tuberculosis mycobacteria | NO | YES |
| Set interpretation criteria | NO | YES |
QFT-Plus streamlines healthcare worker TB control programs.
Replacing the skin test with QFT-Plus provides reduced on-boarding time and accurate exposure testing while improving surveillance quality and efficiency.
Healthcare workers are at increased risk of tuberculosis infection
Hospitals, clinics, and other congregate health settings are well recognized as areas of potential TB transmission. The transmission of TB of any kind (e.g., patient to worker, worker to worker, or worker to patient) within a healthcare setting can have significant consequences for healthcare operations, which is why many countries and institutions recommend or mandate regular surveillance of TB infection status among health care workers. Pre-employment and regular, ongoing screening for TB infection of doctors, nurses, custodial staff, and other health professionals help institutions monitor potential for occupational TB exposure and future infection. Implementation of targeted TB screening in groups with higher risk of exposure, such as healthcare workers, contributes significantly to effective TB control (2).
The tuberculin skin test may be insufficient in a healthcare setting
Besides the second appointment needed for test reading, the tuberculin skin test (PPD or TST) has several disadvantages. Cross-reactivity with non-tuberculous mycobacteria and – for healthcare workers even more important – the cross-reactivity with the Bacille Calmette-Guérin (BCG) vaccine are responsible for the low specificity of the skin test. In some countries that have ceased BCG vaccination in the general population, healthcare workers are still vaccinated because they are considered a TB risk group. BCG vaccination has a profound impact on skin test results in healthcare worker population (2–5). In addition to the reductions in specificity caused by cross-reaction with BCG and non-tuberculous mycobacteria, repeated intradermal application of the tuberculin might result in an unwanted stimulation of the immune system of the healthcare worker, further lowering the specificity of the skin test in healthcare worker screening (2).
Interpretation of skin test results depends on exposure circumstances and country. In order to circumvent the problem of cross-reactivity with the BCG vaccine, high thresholds for a positive skin test result (>15 mm) are chosen in some countries (e.g., France, Portugal). However, this does not allow for the elimination of the influence of BCG on the skin test and reduces the sensitivity of skin test results (2, 6, 7). In some healthcare worker populations skin test positivity is as high as 70% (e.g., France, Portugal).
QFT-Plus better identifies risk for TB infection in healthcare workers than the skin test
The use of Interferon Gamma Release Assays (IGRAs), like QFT-Plus, is more suited to the healthcare setting than the tuberculin skin test, particularly in countries of low TB burden, due to their high specificity and the potential for reducing costly unnecessary follow-up and treatment. Several studies have demonstrated that IGRAs, particularly QFT, have higher specificity over the skin test, principally in countries with low TB burden (8). In a metaanalysis, IGRA results were observed to be well correlated with TB infection risk factors, including occupational exposure, such as a healthcare worker's presence in a high-risk ward, TB clinic, or geriatric ward (9). Compared with the skin test, QFT demonstrates the highest specificity for TB infection (99.2%) in the general population in low TB prevalence settings (10). The use of QFT instead of the skin test would save between 25 to 98% of the chest x-rays needed to exclude active TB after a positive skin test.
To date, research indicates that the newest QuantiFERON TB test, QuantiFERON-TB Gold Plus (QFT-Plus), has shown good correlation and performance compared to its predecessor, QuantiFERON-TB Gold (QFT, 10), with publications on sensitivity (11–13), specificity (13, 14), utility in monitoring treatment (15), and importantly performance in healthcare workers (14). Like its predecessors, a positive QFT result correlates better to TB risk and is a better predictor of true infection from M. tuberculosis compared to the skin test (13).
Global migration increases the burden of latent TB infection
Tuberculosis is a truly global issue, especially in a healthcare setting. Migration from high TB burden countries to more developed, low TB burden countries can jeopardize infection control success. The prevalence of latent TB infection in migrants from high TB burden countries is high, and the risk of reactivation during the first years after migration is elevated (16). Therefore, TB risk in patients with a migration background is increased, yielding a potential source of infection for healthcare workers. Furthermore, migrating healthcare workers might import TB into the healthcare system of the host country. This stresses the need for pre-employment and ongoing or serial screening for latent TB infection of healthcare workers (17).
QFT-Plus can provide a more cost-effective approach than the skin test in healthcare settings
Although traditionally perceived as low-cost and simple, several factors drive inefficiency of the tuberculin skin test in the healthcare setting, including: Increased labor costs due to requirement for 2 visits, variable specificity of the skin test, particularly in BCG vaccinated individuals, requirement for specially trained personnel to administer the skin test, high inter- and intra-reader variability. In addition to these programmatic inefficiencies, due to its low specificity particularly in low prevalence populations with a mixed BCG vaccination status, the skin test is associated with other potential costs such as follow-up physician visits, unrequired antibiotic treatments, and chest x-rays. Several studies demonstrated that introducing interferon-gamma release assays, like QFT-Plus, to support TB screening of healthcare workers will improve the cost-effectiveness of the screening program (18–21).
.
Want to learn more about streamlining your healthcare worker testing with QuantiFERON-TB Gold Plus?
Contact a QFT-Plus expertReferences
1. Baussano, I., et al. (2011) Tuberculosis among health care workers. Emerg. Infect. Dis. 17, 488.
2. Costa, J.T., et al. (2009) Tuberculosis screening in Portuguese healthcare workers using the tuberculin skin test and the interferon-gamma release assay. Eur. Respir. J. 34, 1423.
3. Nienhaus, A., Schablon, A., Le Bacle, C., Siano, B., and Diel, R. (2008) Evaluation of the interferon-γ release assay in healthcare workers. Int. Arch. Occup. Environ. Health 81, 295.
4. Tripodi, D. et al. (2009) Evaluation of the tuberculin skin test and the interferon-gamma release assay for TB screening in French healthcare workers. J. Occ. Med. Tox. 4, 30.
5. Harada, N., Nakajima, Y., Higuchi, K., Sekiya, Y., Rothel, J., and Mori, T. (2006) Screening for tuberculosis infection using whole-blood interferon-gamma and Mantoux testing among Japanese healthcare workers. Infect.Control Hosp. Epidemiol. 27, 442.
6. Moucaut, A. et al. (2013) The effect of introducing IGRA to screen French healthcare workers for tuberculosis and potential conclusions for the work organization. J. Occ. Med. Tox. 8, 12.
7. Nienhaus, A., Ringshausen, F.C., Costa, J.T., Schablon, A., and Tripodi, D. (2013) IFN-γ release assay versus tuberculin skin test for monitoring TB infection in healthcare workers. Expert. Rev. Anti. Infect. Ther.11, 37.
8. ECDC European Centre for Disease Prevention and Control (2011) Guidance for the Use of interferon-gamma release assays in support of TB diagnosis. Stockholm. doi: 10.2900/38588.
9. Zwerling, A., van den Hof, S., Scholten, J., Cobelens, F., Menzies, D., and Pai, M. (2012) Interferon-gamma release assays for tuberculosis screening of healthcare workers: a systematic review. Thorax 67, 62.
10. QuantiFERON-TB Gold Plus (QFT-Plus) Package Insert, Rev. 04. February 2016.
11. Hoffmann, H., et al. (2016) Equal sensitivity of the new generation QuantiFERON-TB Gold plus in direct comparison with the previous test version QuantiFERON-TB Gold IT. Clin. Microbiol. Infect. 22, 701.
12. Yi , L., et al. (2016) Evaluation of QuantiFERON-TB Gold Plus for detection of Mycobacterium tuberculosis infection in Japan. Sci. Rep. 6, 30617.
13. Barcellini, L., et al. (2016) First Independent Evaluation of QuantiFERON-TB Plus Performance. Eur. Respir. J. 47,1587.
14. Moon, H et al (2016) Evaluation of QuantiFERON-TB Gold Plus in Healthcare Workers in a Low-Incidence Setting, J. Clin. Microbiol. 55,1650.
15. Kamada, A., Amishima, M. (2017) QuantiFERON-TB® Gold Plus as a potential tuberculosis treatment monitoring tool. Eur. Respir. J. 49, 1601976.
16. Liu, Y. et al. (2012) Estimating the Impact of Newly Arrived Foreign-Born Persons on Tuberculosis in the United States. PLoS ONE 7, e32158.
17. Horsburgh C.R., and Rubin E.J. (2011) Clinical practice. Latent tuberculosis infection in the United States. N. Engl. J. Med. 364, 1441
18. Eralp, M.N., Scholtes, S., Martell, G., Winter, R., and Exley, A.R. (2012) Screening of healthcare workers for tuberculosis: development and validation of a new health economic model to inform practice. BMJ Open 2, e000630
19. de Perio, M., Tsevat, J., Roselle, G.A., Kralovic, S.M., and Eckman, M.H. (2009) Cost-effectiveness of Interferon Gamma Release Assays vs Tuberculin Skin Tests in Health Care Workers. Arch. Intern. Med 169, 179.
20. Nienhaus, A., Schablon, A., Costa, J.T., and Diel, R. (2011) Systematic review of cost and cost-effectiveness of different TB-screening strategies. BMC Health Serv. Res. 11, 247.
21. Pareek, M. et al (2011) Screening of immigrants in the UK for imported latent tuberculosis: a multicentre cohort study and cost-effectiveness analysis. Lancet Infect. Dis. 11, 435.