お問い合わせ
-
各種お問い合わせはこちらから www.quantiferon.com/jp/contact-us/

One in 3 people in the world are infected with latent TB (LTBI), with a 10% average lifetime risk of developing active TB (1). The conversion from LTBI to active TB disease can occur as a result of the immune system being significantly compromised. HIV infection is the biggest known risk factor for reactivation of LTBI (Figure 1).
Therefore, early identification and early treatment of LTBI can have a significant impact on the health outcomes of individuals infected with HIV.
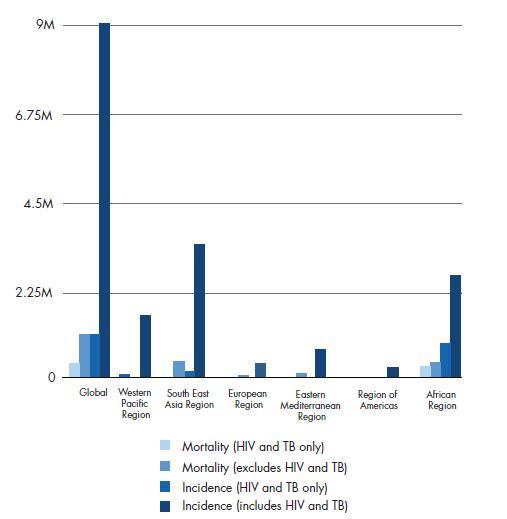
Figure 1. Global estimated epidemiological burden of TB (2).
Previously, the only tool available for identifying LTBI was the tuberculin skin test (TST), or Mantoux test. The TST is an in vivo test that measures immune responses to tuberculin purified protein derivative (PPD), which is made up of a multitude of bacterial proteins. Most of these proteins are present in the BCG vaccine, and shared with many environmental mycobacteria. As such, immunological reactions to the PPD reagent used in the TST may be nonspecific and may contribute to increased rates of false-positive results (8). IGRAs offer a new paradigm in diagnosing TB infection. QFT is the most clinically tested and proven IGRA, with over 1000 peer-reviewed, published clinical papers.
A variety of factors, other than TB infection, are known to induce a false-positive TST result. These include BCG vaccination, exposure to NTM, the inherent boosting effects of prior TST testing, and subjectivity and variability (intraobserver and inter-observer) when reading test results (8–9). Decreased specificity has been shown to occur in those who have been BCG vaccinated. False-positive results often lead to unnecessary treatment for TB infection with possible detrimental side effects (10). False-negative results are also a common limitation of the TST (11). The TST is unable to distinguish between anergic reactions and negative results. Following the initial intradermal injection of PPD, recipients are required to return within 72 hours to permit reading of the result. Failure to return for TST reading, often in the range of 30-50% of those tested, is common in HIV-infected populations, thereby undermining the sensitivity of TST and increasing the costs of screening (12–14).
HIV-positive individuals are at risk of progressing to active TB disease and outbreaks, due to the combination of immune suppression from HIV and population risks such as homelessness, incarceration and drug use (15).
Both NPV and PPV are heavily dependent on the prevalence of infection in the population being tested. In most developed countries, the prevalence of M. tuberculosis infection is relatively low. The largest study in a low-endemic region is by Aichelburg et al., who studied the PPV of QFT longitudinally in 830 HIV-positive individuals. Of the 37 who were QFT-positive/HIV positive, 3 (8.1%) developed active TB during the follow-up period of 19 months. None of the 793 QFT-negative individuals progressed to active TB, indicating an excellent NPV, in this case, an NPV of 100%. One important limitation of the Aichelburg et al. data is the relative scarcity of study individuals with very low (<200) CD4+ cell counts. There is a high likelihood that individuals with such low CD4+ cell counts, and infected with MTB, would have already progressed to active disease and these individuals would be excluded from this study and therefore the results (10). In a similar study, Soborg et al. conducted a 6 year follow-up study on HIV-positive patients in Denmark. QFT accurately identified all those tested who would progress to active TB, and no one who was QFT-negative developed TB (16) (Figure 2).
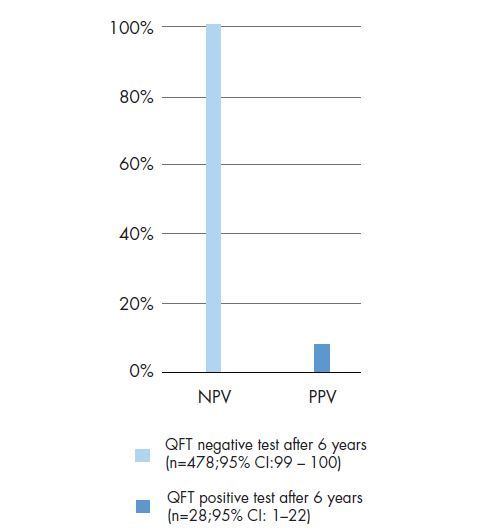
Figure 2. QFT Negative/Positive Predictive Value in HIV cohort (16)
A large number of studies have analyzed QFT performance in individuals living with HIV. Some studies have shown that the sensitivity of QFT in HIV co-infected individuals is impaired compared with HIV-negative patients with TB disease, although to a lesser degree than the TST (3).
A significant benefit of QFT over the TST is that it incorporates a positive control (15). However, like the TST, QFT relies on functional CD4+ cells, and its performance can be negatively influenced by low and impaired CD4+ cell counts in HIV-infected individuals (16). Unlike the TST, the positive control of QFT provides an indicator of the overall immune function. An indeterminate QFT result in an HIV-infected person with a low CD4+ cell count can provide valuable information. It suggests possible anergy and does not necessarily indicate a failed test (17, 18) (Table 1).
| CD4 count | Indeterminate QFT result* |
|---|---|
| CD4<100 | 16.1% |
| CD4 100-350 | 3.6% |
| CD4>350 | 3.9% |
* All indeterminate results were due to a failure to respond adequately to the positive control.
A positive QFT result indicates the person tested is likely infected with M. tuberculosis. The individual with a positive QFT result should have a medical evaluation that includes a symptom review, risk factor assessment, chest x-ray and physical examination to determine the diagnosis of active TB or LTBI.
Numerous studies have investigated the use of QFT in HIVpositive populations. The characteristics of these studies are outlined in the QFT HIV Clinical Guide, which can be downloaded below. Of note is that QFT has been shown to have equal or higher sensitivity when compared with the TST. Perhaps the biggest disadvantage of the TST is that it lacks an internal control to distinguish false negative results due to anergy from true negative results.
References
1. World Health Organization (WHO). Tuberculosis Fact sheet No.104 Updated October 2015. http://www.who.int/mediacentre/factsheets/fs104/
2. World Health Organization (WHO). Global Tuberculosis Report 2014. http://apps.who.int/iris/bitstream/10665/137094/1/9789241564809_
eng.pdf. Accessed July 27 2015.
3. Kwan, C.K. and Ernst, J.D. (2011) HIV and tuberculosis: a deadly human syndemic. Clin. Microbiol. Rev. 24, 351–376.
4. Golub., J.E. et al. (2007) The impact of antiretroviral therapy and isoniazid preventive therapy on tuberculosis incidence in HIV-infected patients in Riode Janeiro, Brazil. AIDS 21, 1141-1148.
5. Badri, M., Wilson, D. and Wood, R. (2002) Effect of highly active antiretroviral therapy on incidence of tuberculosis in South Africa: a cohort study. Lancet 359, 2059-2064.
6. Lawn, S.D., Badri, M. and Wood, R. (2005) Tuberculosis among HIV-infected patients receiving HAART: long term incidence and risk factors in a South African cohort. AIDS 19, 2109-2116.
7. Girardi, E. et al. (2005) Incidence of Tuberculosis among HIV-infected patients receiving highly active antiretroviral therapy in Europe and North
America. Clin. Infect. Dis. 41, 1772-1782.
8. Centers for Disease Control and Prevention. (2010) Centers for Disease Control and Prevention. Updated guidelines for using interferon gamma
9. QuantiFERON-TB Gold (QFT) ELISA Package Insert. Please consult the current online version for your country at www.QuantiFERON.com.
10. Aichelburg, M.C. et al. (2009) Detection and prediction of active tuberculosis disease by a whole-blood interferon-γ release assay in HIV-1–infectedindividuals. Clin. Infect. Dis. 48, 954–962.
11. Ramos, J.M. et al. (2012) Contributions of an interferon-gamma release assay testing to the diagnosis of latent tuberculosis infection in HIV-infected patients: A comparison of QuantiFERON-TB Gold In Tube, T-SPOT.TB, and tuberculin skin test. BMC Infect. Dis. 12, 169.
12. Cheallaigh, C.N. et al. (2013) Interferon gamma release assays for the diagnosis of latent TB infection in HIV-infected individuals in a low TB burden country. PLoS One.8(1), e53330.
13. Chaisson, R. E., Keruly, J.C., McAvinue, S., Gallant, J.E. and Moore, R.D. (1996) Effects of an incentive and education program on return rates for PPD test reading in patients with HIV infection. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 11, 455-459.
14. Malotte, C. K., Rhodes. F. and Mais. K.E. (1998) Tuberculosis screening and compliance with return for skin test reading among active drug users. Am. J. Public Health 88, 792-796.
15. Jones, S., de Gijsel, D., Wallach, F.R., Gurtman, A.C., Shi, Q. and Sacks, H. (2007) Utility of QFT testing for latent TB infection in HIV-infected individuals. Int. J. Tuberc. Lung Dis. 11, 1190–1195.
16. Soborg, C., Ruhwald, M., Andersen, P.H. and Ravn, P. (2014) 6-year follow-up of 522 HIV-positive individuals screened for Mycobacterium tuberculosis infection in Denmark. Eur. Respir. J. 44, 540–543.
17. Hoffmann, M. and Ravn, P. (2010) The use of interferon-gamma release assays in HIV-positive individuals. Eur. Infect. Dis. 4, 23–29.
18. Luetkemeyer, A.F. et al. (2007) Comparison of an interferon-gamma release assay with tuberculin skin testing in HIV infected individuals. Am. J. Respir. Crit. Care Med. 175, 737–742.
Product claims may differ from country to country based on regulations and approvals. Contact your country representative for further details.
各種お問い合わせはこちらから www.quantiferon.com/jp/contact-us/